|
| Prof. Dr. Gunther Deuschl |
 |
| Prof. Dr. Olaf Jansen |
The
The following is an inquiry received from Prof. Dr. Günther Deuschl, Chairman of the Department of Neurology, UKSH, Christian-Albrechts University, Kiel, Germany. Please post your ideas on this case in the comments section:
Dear friends,
I
have a patient presenting with different noises: one subjectively in
the thyroid region (nothing objectively), one in the region of the ear
(coming erratically in groups, some resemblance to earclicks, again
nothing objectively), one pulse synchronous noise (with a known
neuroradiologically confirmed and treated fistula carotis to sinus
cavernosus). I would have considered her to have only the latter
clinical problem. All the other complaints seemed to be due to enhanced
introspection without definite psychiatric diagnosis. Then the
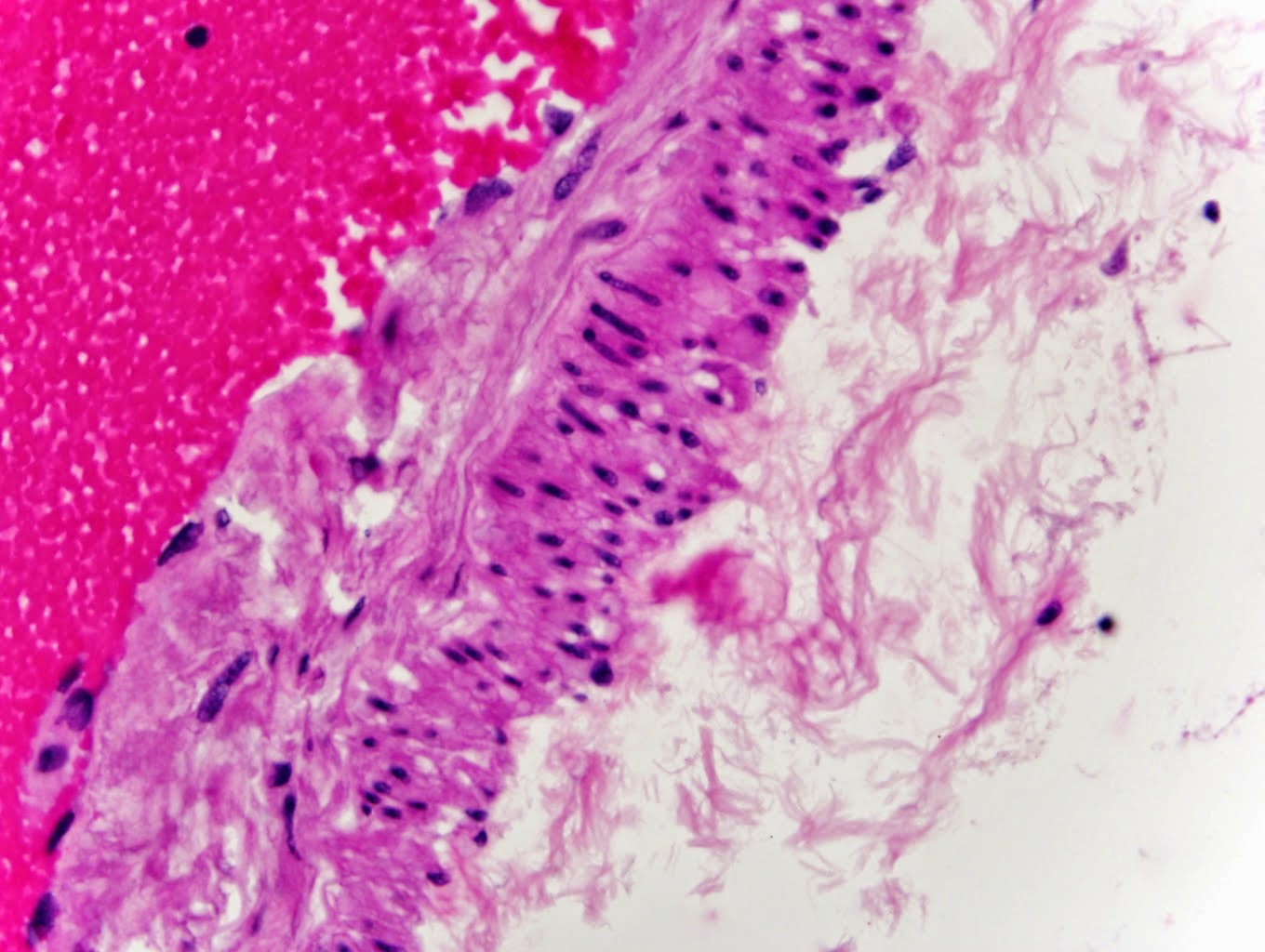
neuroradiologist (Prof. O. Jansen, Kiel University, Germany) made an MRI
scan and found this curious ‘Tic-sign’ of the brain stem (you will
understand when you look at the images below, which you can click on to
enlarge). It shows definite circumscribed regional and bilateral atrophy
of the inferior olive. Interestingly there seems to be some ‘white
matter’ remaining. . Indeed an olivary agenesis or dysgenesis is one of
the possibilities. The lady has no cerebellar signs as you see this
sometimes (but not always) after olivary destruction.
I wonder if anybody has ever seen something like this and have an insights on a diagnosis?
Best regards for taking your time to read and see this.
Guenther